Before going to explain “HOW DO ANTIBIOTICS WORK TO KILL BACTERIA” we should know the structure of bacteria.
Why? Is it necessary?
Yes, extremely important because it is the structure (cell wall) that is disrupted by antibiotics.
Okay.
So how is the structure of a bacteria?
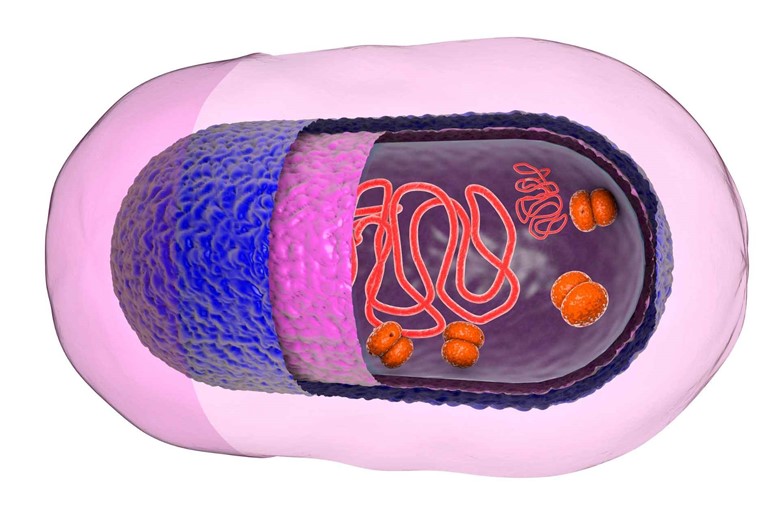
Bacteria have a cytoplasmic membrane that covers the protoplasm of the bacteria and outside the cytoplasmic membrane, there is an important structure of bacteria i.e cell wall.
Why cell wall is important?
Because it is the structure where antibiotics work.
Could you please explain the structure of the cell wall of the bacteria?
Yes sure.
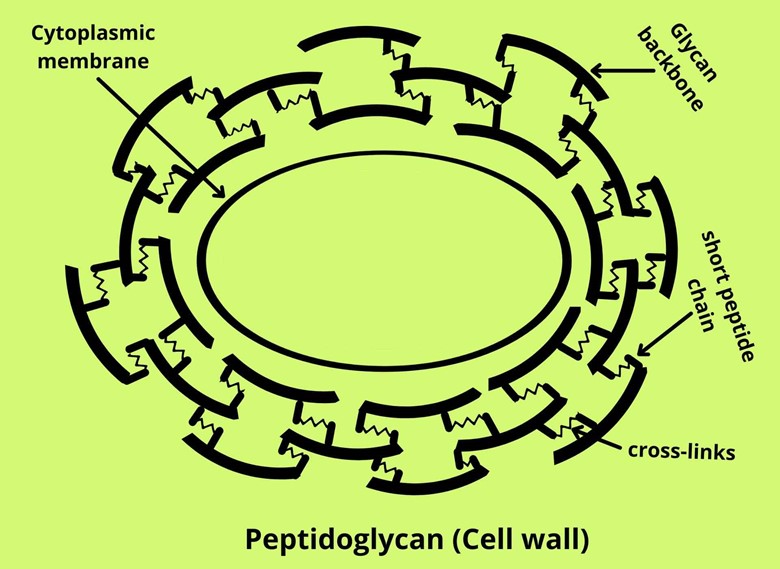
The cell wall of bacteria is made up of a sugar backbone called glycan which is linked by a short chain of amino acids (about 4 to 5 amino acids) called peptides. The short-chain is then cross-linked with each other and the whole structure is called peptidoglycan.
Here a question that arises is how many molecules of peptidoglycan are present in a cell wall of bacteria?
Well, that looks like a valid and good question.
The answer is that this peptidoglycan is a single macromolecule so the bacteria have one single macromolecule of peptidoglycan in their cell wall.
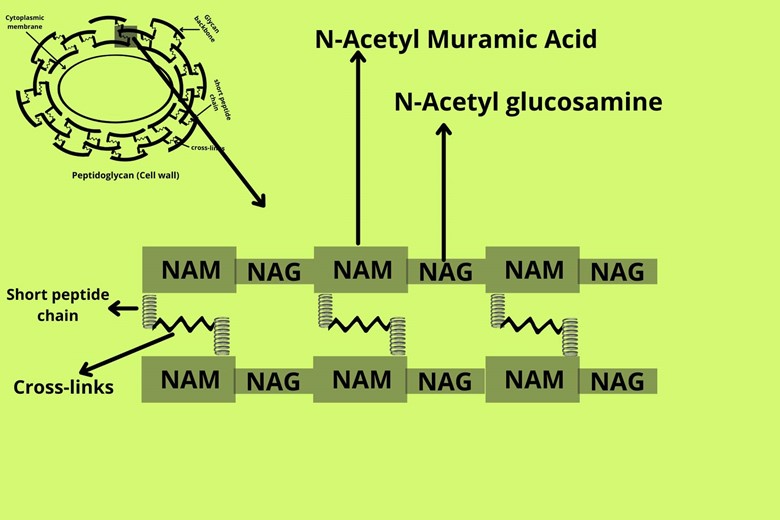
Let’s go into more detail about peptidoglycan. If we zoom the glycan backbone of the bacterial cell wall it is made up of two sugar units i.e N-acetyl muramic acid (NAM) and N-acetyl glucosamine (NAG). These two units are repeated again and again in the glycan backbone of the bacterial cell wall. The short chains of amino acids (peptides) are attached to the NAM unit of the glycan backbone which is then cross-linked with each other.
But what is the function of peptidoglycan in bacterial cell walls?
The cell wall of bacteria prevents the bacteria from osmotic burst or cytolysis. An osmotic burst is a phenomenon in which the water moves from the bacterial outside hypotonic environment to inside hypertonic environment which causes the content of bacteria to exert pressure on the membrane of bacteria called turgor pressure, in the same time the membrane of bacteria also exert equal and opposite pressure on the cell called wall pressure when the turgor pressure exceeds the turgor pressure then the cell burst, this phenomenon is called osmotic burst.
So antibiotic kills bacteria by osmotic burst?
Before going to this first we have to know how the cell wall form because different drugs and antibiotics work differently by preventing the formation of the bacterial cell wall. The action of different drugs acting is described below.
I) Cycloserine:
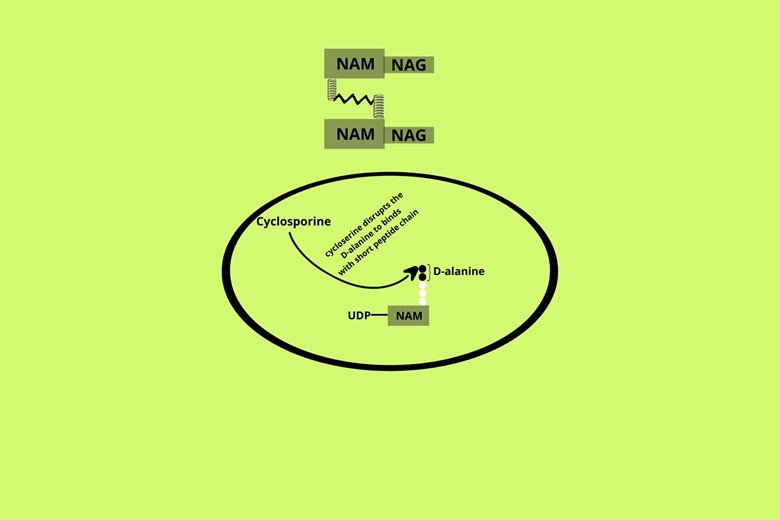
Inside the cytoplasmic membrane, the glycan units i.e NAG and NAM monosaccharides units are carried by a carrier molecule called Uradin diphosphate (UDP). The short peptide chain is attached to the NAM unit. The last amino acids of the short-chain (about 4 to 5 amino acids) are D-alanine (also called S-alanine)
The cycloserine disrupts the D-alanine to bind with the short peptide chain so it means that in the presence of cycloserine the NAM unit didn’t get the proper formation of a short peptide chain. So when this improper unit is secreted for cell wall formation it will not make proper cross-links and there will be no formation of the cell wall.
II) Bacitracin:
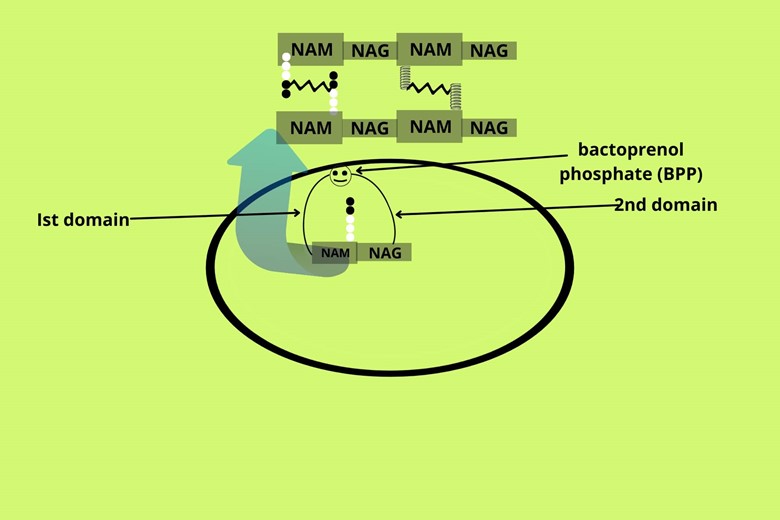
If cycloserine doesn’t available or it didn’t work then there is another choice of drug available that can prevent bacterial wall synthesis. The cytoplasmic membrane of the bacteria contains a protein called bactoprenol phosphate (BPP) that holds the NAM unit with a short peptide chain in one domain and the NAG unit in another domain and fuses them. The NAM with peptide chain and NAG are called repeat units. The bactoprenol phosphate (BPP) transfers the intracellular repeat units to the extracellular environment where it attaches to the preexisting glycan backbone through a glycosidic bond for cell wall synthesis. The bactoprenol phosphate (BPP) will again take another repeat unit and will transfer again outside until the cell wall is formed.
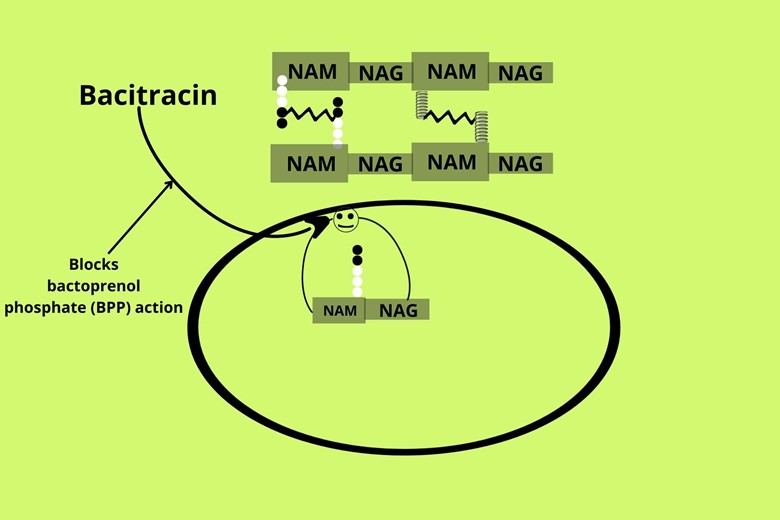
The drug group bacitracin binds with bactoprenol phosphate (BPP) and does not allow it to come back to the intracellular environment once it moves out with a repeat unit and in this way the cell wall synthesis is blocked and prevented.
III) Vancomycin:
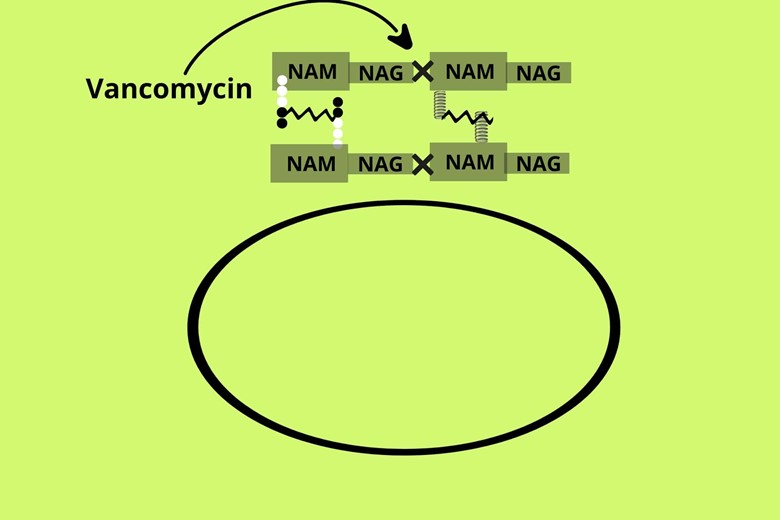
The third step in cell wall synthesis is the combination of secreted repeat units (NAM with peptide chain and NAG unit) with the pre-existing glycan backbone so if the patient is not exposed to cycloserine and Bacitracin then we have the third choice of drugs i.e Vancomycin. The Vancomycin does not allow the attachment of secreted repeat units with pre-existing glycan backbone which results in the prevention of synthesis of the cell wall of bacteria and exposing them to the osmotic burst.
IV) Penicillin and Cyclosporin:
If the NAM with a short peptide chain is normally synthesized i.e normal D-alanine it is normally transported with NAG outside and it attaches normally with the previous existing glycan backbone still we have a chance to prevent and weaken the bacterial cell wall.
How?
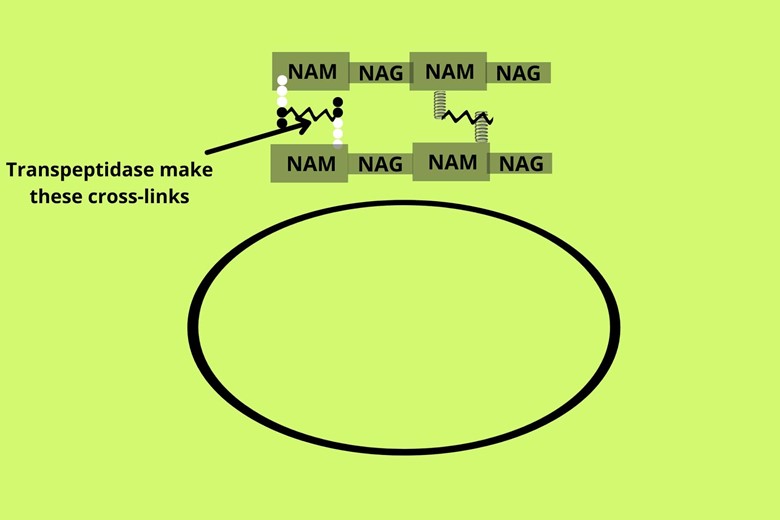
There is an enzyme called transpeptidase that makes the cross-links between peptides of the NAM of the cell wall.
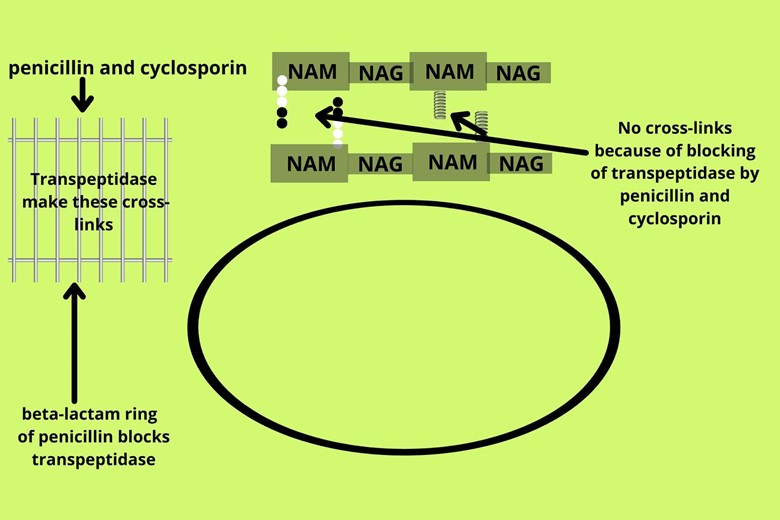
So if the newly synthesizing bacteria are exposed to penicillin and cyclosporin antibiotics it will prevent the cross-links of peptide chains of NAM with each other so if there are no cross-links between the peptide chain of the NAM units then there will be no or weak synthesis of the cell wall. The Penicillin goes to the cytoplasmic membrane where its beta-lactam ring inhibits the transpeptidase enzyme of bacteria
which makes the cross-links between the peptides of the cell wall so that the wall doesn’t form and water starts entering until the osmotic burst occur.
But I have heard that bacteria cell walls are in continuous remodeling how do antibiotics prevent them?
That’s a good question. Normally when new synthesis goes on, a little lysis also occurs for which there is an enzyme called autolysin in bacteria that destroy the old cell wall and transpeptidase makes the new cell wall but as discussed the transpeptidase was blocked by penicillin and cyclosporin so the new cell wall will form very weak while the autolysin is not inhibited by antibiotic so the destruction continues until cell wall doesn’t form and water moves inside due to which osmotic burst will happen because the cell wall cannot keep their integrity.
But if the bacteria has a well-formed cell wall then how it will be killed?
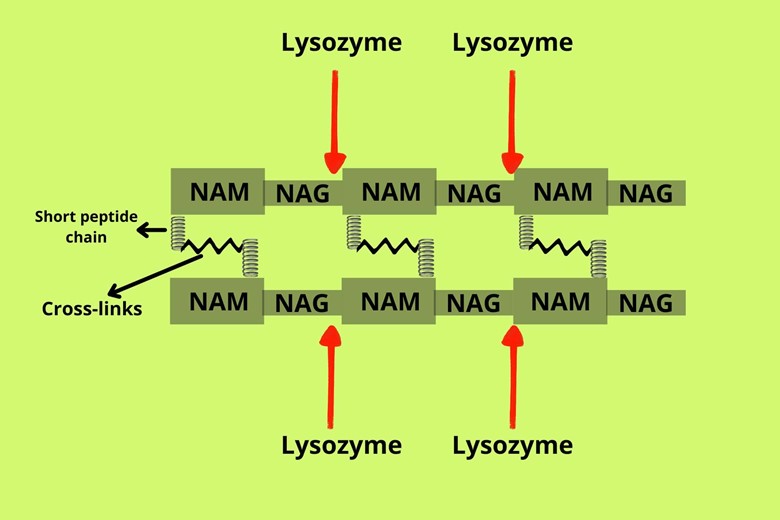
As you know that our body contains trillions of bacteria that can cause disease if get any opportunity. But the tears, saliva, and mucosal secretions of our body contain a natural enzyme called lysozyme which breaks the NAM and NAG units of the glycan of the already-formed cell wall of bacteria so we are protected by natural immunity.
But how do antibiotics work without harming the surrounding human cells?
The answer to this question is that the antibiotic has target molecules where it binds and destroys them as we discussed earlier the different ways of action of different antibiotics (i.e Cycloserine, Bacitracin, Vancomycin, Penicillin, and Cyclosporin). Also, here we can say that bacteria have cell wall while the human doesn’t have cell wall so the human cells are not affected by the antibiotics.
We didn’t talk about gram-positive and gram-negative bacteria and the action of the antibiotics on them?
For this, we have to know the structure of these bacteria.
The one which we discussed earlier, is which one?
The earlier discussed bacteria are gram-positive bacteria. But there is one more molecule in gram-positive bacteria i.e teichoic acid (polymer of ribitol phosphate or glycerol phosphate) which helps in adherence of bacteria and activates the macrophages to release a lot of interleukin-1 and tumor necrotic factors. The drug or antibiotic action we discussed earlier.
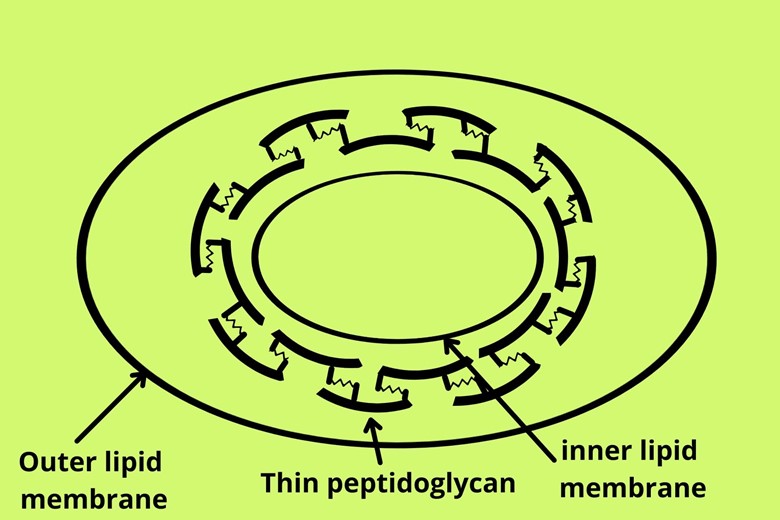
Coming to the gram-negative bacteria, first, we have to understand their structure, and then we will discuss the antibiotic action on it. Outside the lipid membrane, (cytoplasmic or cell membrane) of the gram-negative bacteria has very thin peptidoglycan while gram-positive bacteria have very dense peptidoglycan backbone with very close cross-links. But the gram-negative bacteria have an additional lipid bilayer outside the peptidoglycan (cell wall) backbone.
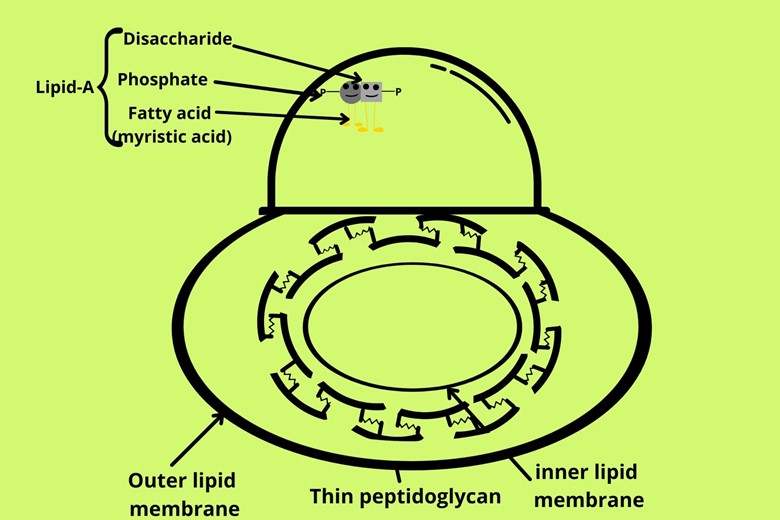
The inner leaf and side of the outermost lipid bilayer have the same phospholipids as the inner lipid bilayer but the outer lead and side of the outermost lipid bilayer have special molecules i.e disaccharide with two phosphate and myristic acid (fatty acid). The disaccharide with two phosphate and fatty acid makes a phospholipid complex called lipid A.
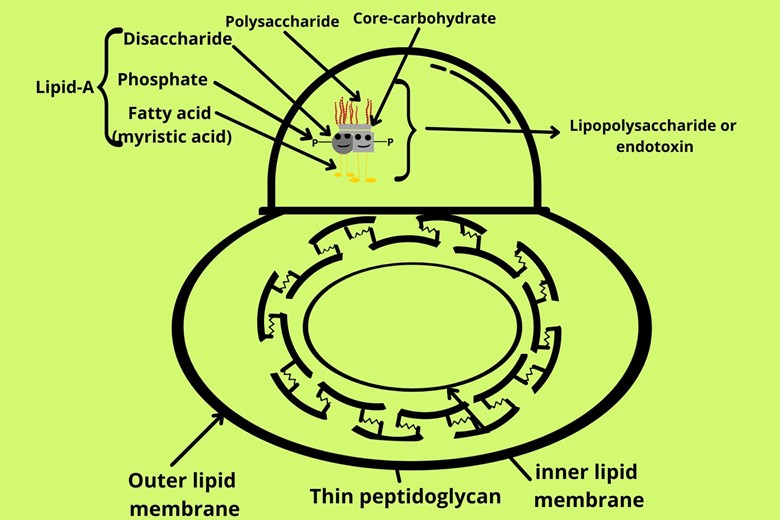
Above lipid A complex there is a molecule of carbohydrate called core carbohydrate and above core carbohydrate, there is another molecule of polysaccharide. The whole complex forms lipid A with core carbohydrates and polysaccharides called lipopolysaccharide or endotoxins. This endotoxin is very dangerous and is the most common cause of death in the ICU.
As discussed that gram-negative bacteria have an additional outer lipid bilayer which provides an additional barrier to the movement of the molecules due to this nature has provided a special type of channel called porin for the transport of molecules from the outer lipid bilayer.
This additional outer lipid bilayer also makes the inner cytoplasm of gram-negative bacteria makes them less accessible to drugs. Initially, penicillin discovered was called G-penicillin because it was effective against gram-positive bacteria and not against gram-negative because the G-penicillin molecules were large and couldn’t pass through the porin of the outer membrane of gram-negative bacteria. Then the doctors and scientists make a new generation of smart molecules penicillin called extended-spectrum penicillin which can attack gram-negative bacteria as well as Gram-positive bacteria. The extended-spectrum antibiotics contain mezlocillin, ticarcillin, carbenicillin, and piperacillin.
Conclusion/Summary:
So it is concluded from the discussion that the cell wall is the main protecting agent against bacterial infection if we disrupt cell wall synthesis or destroy the already made cell wall of bacteria then there will be movement of water from outside to inside bacteria until the osmotic burst occurs. The water moves inside because bacteria have an inner hyper-concentrated environment. Antibiotics like Cycloserine, Bacitracin, Vancomycin, Penicillin, and Cyclosporin prevent and disrupt cell wall synthesis by blocking different synthetic ways due to which the newly formed bacterial cell wall is weak and cannot maintain its integrity so that the water moves inside until osmotic burst happen.




2 thoughts on “How Do Antibiotics Work to Kill Bacteria?”
I really like looking through an article that can make people think. Also, thank you for allowing me to comment!
Welcome.