One might think the answer to “What is the difference between gingivitis and periodontitis?” is the same, but there is a difference between these two diseases. These diseases, i.e., gingivitis and periodontitis, are real headaches for people, but this can be stopped before they get caught. Here in this article, I am giving a detailed description of gingivitis and periodontitis, their causes, effects, and treatment. After reading this article, you will have no confusion about these two diseases. And for prevention or treatment, check out the Top 10 best toothpaste for gingivitis and bleeding gums.
These diseases start with teeth and gums, so let’s start by explaining the structure of teeth and gums.
What are teeth?

Teeth can be defined as:
“Hard calcified projection from gums used for mastication of food and offense and defense purposes in humans as well as in many vertebrates.”
The term “gum” what is meant by this?
Well, wait, please. First, we should go for the tooth structure, and then we will come to the gums.
Did you look at yourself smiling in the mirror?

Yes, there is nobody who has not seen their tooth except blinds.
What have you seen?
The white hard part and the soft part are where the tooth projects.
Well, the tooth has three parts.
I) Crown:

The white and visible part you see is the crown.

The crown is made up of a hard white layer called enamel. Enamel is the hardest part of the body.
Why are enamels so hard?

Good question, Because it is made up of mineral material (96%), non-living tissue, i.e., hydroxyapatite, and water (2–3%). Hydroxyapatite is crystalline calcium phosphate, So take care of your teeth because it cannot be built up naturally.
I think you are clear now about enamel.
Yes, pretty clear.
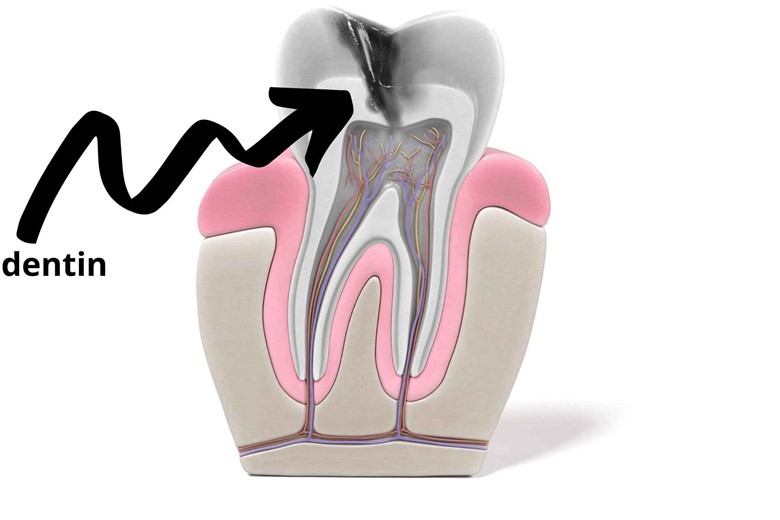
Below the enamel, there is another layer called dentin. It forms the bulk of the teeth. But it is not as hard as enamel.
Pulp:
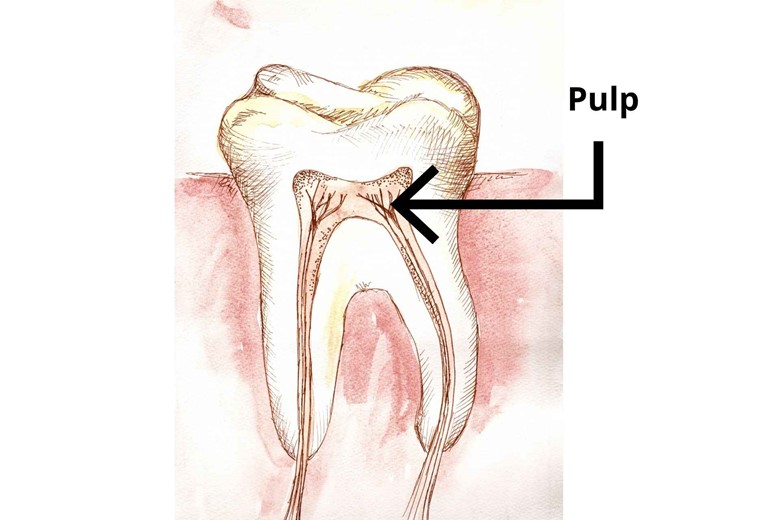
The soft part of dentin is called the pulp. Here, blood vessels and nerves reside.
So what is the function of pulp then?
It has:
- Sensory function
Did you feel pain in your teeth?
Yes.
And did you detect the temperature and pressure change by your teeth?
Yes. That’s the pulp that detects these changes.
- Dentin formation
The pulp is the structure that forms dentin.
- Nourishment
Finally, teeth also need nourishment and moisturization, which blood vessels in pulp provide.
Is the teeth’ color related to enamel or dentin?

It depends on both enamel and dentin.
How?

Firstly, the teeth’ color is determined by dentine, which tends to be yellowish, and then by the enamel translucency.
If the enamel is more translucent then more light will pass through the enamel reflecting the purer color of dentin.
The less translucent, the more light will reflect by enamel and will show whiter color.
But we didn’t hear about Root?
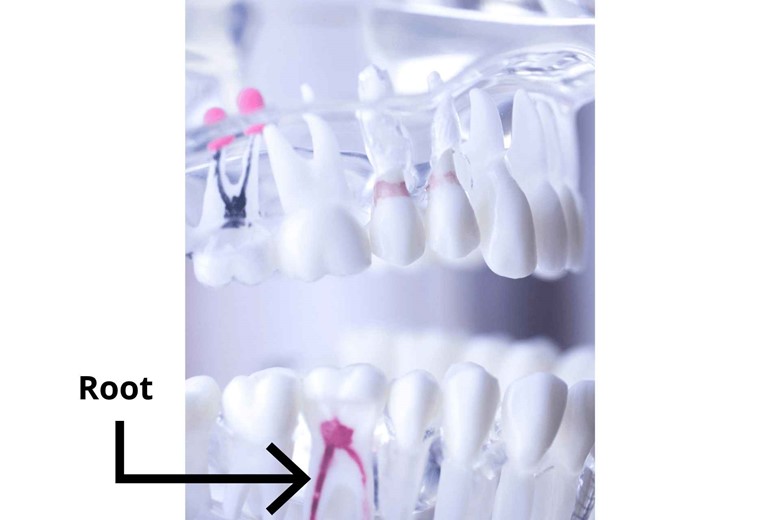
Root is that part of teeth that is invisible and embedded in gums (explained later in this article).
Can you please tell us the function of the root?
Of course, roots anchor the teeth inside the bone.
Have you heard about the alveolar process?
No.
Don’t worry; I am making it clear here.

The alveolar process is a thickened ridge on the jaw bone that contains the socket to hold teeth. These bones are the maxilla (upper jaw bone) and mandible (lower jaw bone) and you know teeth are present on these bones.
Now I am sure that you are clear about tooth structure!
Yes, pretty clear.
Between these, there is one more structure, i.e., the neck of the teeth.
II) Neck:
Between the crown and root, there is a part called the neck of the teeth, which joins or connects the crown with the root.
Now come to your question, gums?
III) Gums:

It is also called gingiva or gingivae (plural). The pink, fleshy, mucosal tissue surrounds the neck of teeth and covers the alveolar part (mandible and maxilla) of the jaw.
Are there any types of gums?
Yes, there are three types of gums.
i) Marginal gum
ii) Attached gum
iii) Interdental gum
Let’s explain them one by one.
i) Marginal gum

As the name indicates, it is present on the margin at the neck of the teeth in a collar-like fashion. Their width varies from 0.5 to 2.0 mm.
ii) Attached gum
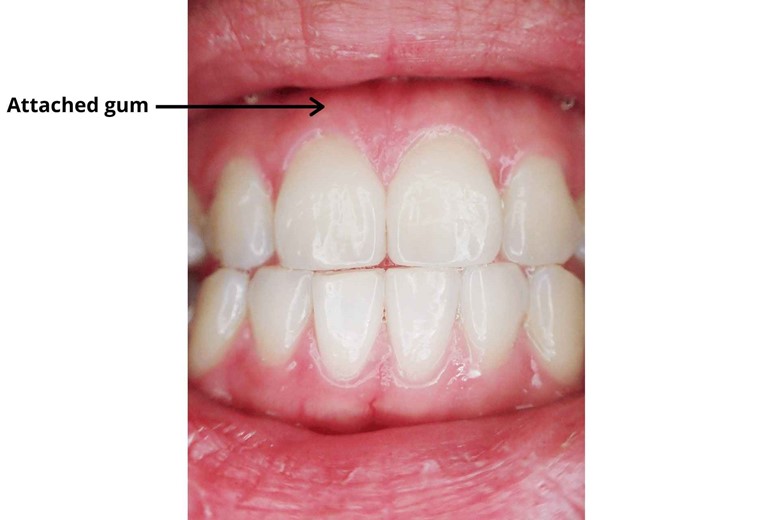
Below marginal gum, there is attached gum, but it is continuous with marginal gum. Their width varies with the location. Generally, it is greater in the incisor region i.e. 3.5mm to 4.5mm in the maxilla (upper jaw bone) and 3.3mm to 3.9mm in the mandible (lower jaw bone).
But their width decreases in the posterior premolar region of the mouth and it ranges from 1.9mm in the maxilla and 1.9mm in the mandible.
iii) Interdental gum
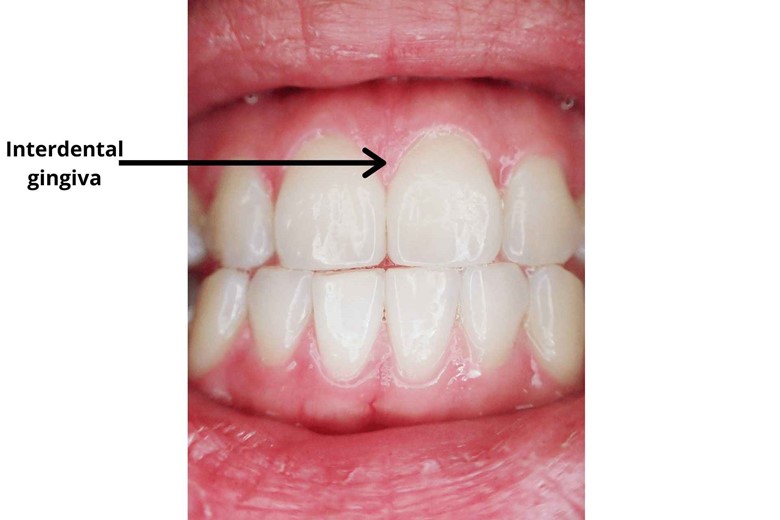
The gum between two teeth is called interdental gum.
There are two more parts of gingiva or gum that I want to explain because they are necessary to understand.
Free gingiva (gum)

The part of the gum that is stuck up and is not anchored to the teeth is called free gingiva.
Gingiva crevice/sulcus
This is the space between the free gingiva and the crown of the teeth.
Are there any signs through which we can identify that our gums are healthy?
Yes, I am giving you some of the signs of your healthy gums.
i) Color

Is your gum color pink, not red or white, not swollen or tender, and does it have limited sensibility to pain, temperature, and pressure?
If yes, then you are lucky you have healthy gums unless you have no other mouth issues.
ii) Counter or shape

Healthy gums have a smooth and scalloped appearance around each tooth. It fills the space between teeth, unlike gingivitis papillae, in which swollen gum papillae fill the space.
iii) Texture

Healthy gums also have a firm texture and often exhibit surface stipplings
iv) Reaction to disturbance

Healthy gums do not show any reaction to common disturbances like brushing or periodontal probing, unlike unhealthy gums that show bleeding, etc.
Clear?
Yes, pretty clear.
Did we move to the next part, gingivitis?
Of course, This is going more interesting.
Okay, let’s dive into it.
Gingivitis

The inflammation of the gums is called gingivitis.
Just that?
No, there is a lot to say about this.
Before going further, let’s explain their types.
I) Drug-induced gingivitis

Certain medications cause an overgrowth of gum tissue known as gingival hyperplasia. The common drugs that do this are immunosuppressants, some calcium channel blockers like Verapamil or Nifedipine, and anticonvulsants.
What are these drugs?
Here, I am giving you a short info about these drugs.
a) Immunosuppressants:
These drugs are anti-rejection drugs. It means it is used to reduce the body’s response to reject the transplanted organ.
b) calcium channel blockers:
Calcium channel blockers are drugs like verapamil or nifedipine, which are used to dilate blood vessels and increase the blood flow and oxygen to the heart reducing the workload.
c) Anticonvulsants:
These drugs are used in the treatment of epileptic seizures (a sudden uncontrollable electrical disturbance in the brain, a neurological disorder) and are also known as antiepileptic drugs or antiseizure drugs.
So if you are using these drugs you can also get gingivitis. To treat this condition just you need to control medication and consult your dentist.
II) Hormonal Gingivitis
Hormonal gingivitis is more common in females than males because they have more hormonal changes during puberty and pregnancy, and using pregnancy birth control pills changes the level of progesterone, which increases blood flow to gums and changes the way gum reacts to an irritant in the plaque, causing gingivitis.
III) Nutritional gingivitis

Nutrition is important for not only the gums but also for the whole body. Severe nutrition deficiency can cause pallor of the gingiva (gums) and heavy bleeding. Controlling nutrients can stop gingivitis.
IV) Plaque-induced gingivitis
This is the most common type of mild gum disease, and as their name shows, gingivitis is due to plaque buildup in the gums or gingiva. The oral unhygienic condition leads bacteria to grow and causes them to red, tender, and bleed.
V) Non-plaque-induced gingival lesions

As the name indicates, this type of gingivitis is due to microorganisms like bacteria, fungi, viruses, etc. Treatment using a mouthwash or consulting your dentist is the best solution.
VI) Acute Necrotizing Ulcerative
This is also known as trench mouth and is a highly painful form of gingivitis, as there are sensitive ulcers between the gum between teeth. This terrible gingivitis is less common than others but the tissue in the gums appears punched out.
Acute necrotizing conditions result due to elevated immune responses and lymph node inflammation.
Signs and symptoms:

- Redness

- Swollen or puffy gums

- Bleeding after brush

- Receding gums

- Tender gums
Do you know there are a lot of bacteria in our mouth?
Yes.
And do you know why this bacteria didn’t cause damage to gums and teeth?
Little, okay, listen, there is a balance of commensal bacteria by immune factors and competition between each other.
Then why does someone get gingivitis?
Dysbiosis.
What is this?

A state of imbalance of bacteria in which pathogenic bacteria increase due to lack of competition by commensal bacteria or by the ineffective immune response.
How do they imbalance?
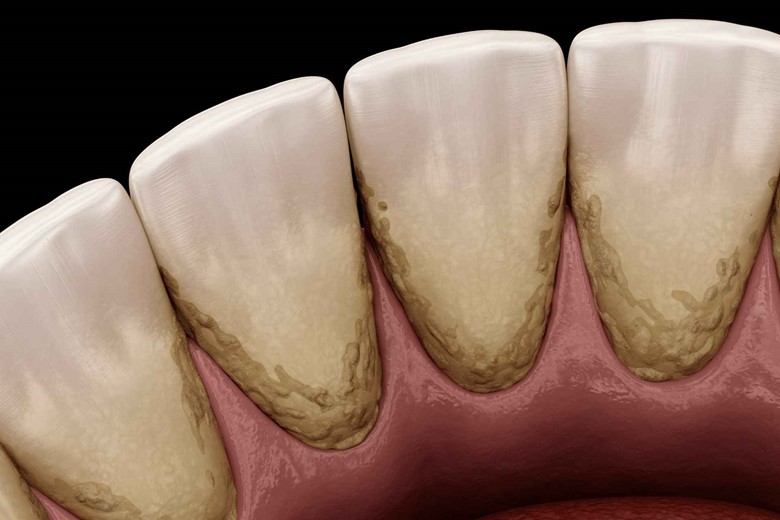
The pathogenic bacteria form dental plaque which is a sticky collection of bacteria, saliva protein, and dead cells of the mouth, and increase their number.
How?
The individual bacteria multiply, form small microcolonies, and form a layer of dental plaque or in other words a biofilm in which bacteria and biofilm communicate with each other through chemical signaling.
So does brushing teeth didn’t remove it?

Well, brushing removes that biofilm on the exposed part of teeth and gums, but some remain in the inner gingiva or gum and invade the inner gums.
And what do they do then?

Damage: as this is their job, the dental plaque then forms a hard mass called dental calculus or tartar. Dental calculus provides a nice space for the bacteria because it is hard and it becomes very difficult to remove it.
This is alarming!
Yes.
Is that going to damage more or stop here?
No, this does not stop until these bacteria satisfy themselves by entering through the gingiva sulcus and causing inflammation which we actually call gingivitis.
But where was that immune system at that time?

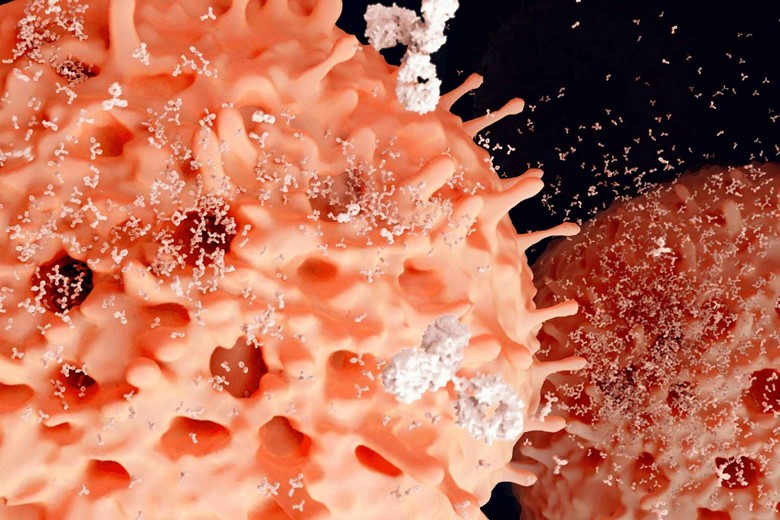
They need signals to work, and damaged gingival cells release inflammatory signals that recruit neutrophils to the damaged area. The neutrophils release harmful chemicals to kill bacteria but these chemicals also damage the nearby tissue.
That’s why you are brushing your teeth or just touching your gums it starts bleeding.
Now, that you understand gingivitis completely, let’s go to their types.
But I have seen some people who take much care of their teeth but still, their gums or gingiva bleeds?
Good question, one of the examinations in patients says that is due to a deficiency of Vitamin D, so if you have this condition then take a high dose of vitamin D and your problem will resolve as it was resolved in patients.
Women in pregnancy have bleeding gums because
During pregnancy, some women’s gums bleed which is also plaque-induced gingivitis, which is due to a hormonal imbalance in which blood flow to the gingiva or gums increases and causes it to be more sensitive, irritable, and swollen.
Also, this hormonal imbalance affects the body’s normal response to the bacteria which can lead to severe conditions.
So how much time a pregnant woman has to bear this problem.
After stopping breastfeeding the hormonal level returns to the normal level stopping more problems with teeth.
Then how can a pregnant woman or up to breastfeeding, have to care for their gums?

Frequent dental cleaning during pregnancy can abate this problem.
Is it reversible to get healthy gums after stopping this disease?
The answer is yes if treated earlier but if conditions get worse then it will lead to an infection called periodontitis.
Periodontitis

The word periodontitis means inflammation around teeth and it is also called pyorrhea which is a Greek word that means “discharge of pus“.
The Pyorrhea/Periodontitis definition is:
“The severe form of gingivitis is in which the gum pulls away from teeth, destroys attachment fibers, and supporting bone that holds the teeth.”

If not treated the ultimate result is the loss of teeth.
When will this condition arise?
When dysbiosis increases more and even more pathogenic bacteria flourish in the mouth. One hypothesis says that the first step in periodontitis formation is the formation of the orange complex of bacteria.
“Orange complex bacteria”
what is it?

The orange complex bacteria serve as a “species bridge” for the early colonizers with highly pathogenic bacteria of the red complex.
Could you please tell us the name of orange complex bacteria and also explain what is red-complex bacteria?

Yes, of course, the orange complex bacteria are gram-negative, anaerobic (can respire in the absence of oxygen) bacteria namely FUSOBACTERIUM NUCLEATUM and PREVOTELLA INTERMEDIA.
Now coming to red-complex bacteria.
Red complex bacteria
These bacteria are highly pathogenic which causes periodontitis. It includes TANNERELLA FORSYTHIA, TREPONEMA denticola, and the most notorious one the PORPHYROMONAS gingivalis.
How does it swell the gingiva which bleeds?
Well, the pathogenic bacteria form a periodontal pocket with the pre-dental plaque. Local mast cell release and nerves trigger the release of histamine which dilates the blood resulting in swelling of the gingiva or gum.
And how lead to tooth loss then?
The damaged gingiva cells release additional cytokines like interleukin-1 which bring more immune cells i.e. neutrophils and macrophages. Ultimate results are again damaging to the gingiva and periodontal ligaments which loosen the tooth.
I want more about PORPHYROMONAS GINGIVALIS?
This bacteria is really damaging bacteria to the gingiva. These bacteria impair immune cells.
Impair immune cells, Kind of shocking, how?
Consider a police station, if the police station of an area is destroyed or controlled by thieves then you should think about the rule of thieves in that area. Similar is the case here, the P.gingivalis destroys or impairs the immune cells and forces other pathogenic bacteria to cause damage.
And how do they get the nutrients?
The immune response delivers more blood flow to the damaged gingiva cells and certainly more nutrients, on which bacteria feed forming a positive feedback process. The positive feedback mechanism instead of stopping increases more and delivers more blood and nutrients, helping more pathogenic bacteria to grow.
It is not the end of the immune system response. The immune response activates the osteoclasts (bone cells) in the bone which dissolve the bone supporting the teeth and even loosen teeth more.
So what is the main cause of this infection and also what are the risk factors?
Generally, the main cause is bacteria but smoking, diabetes, HIV, or AIDS are risk factors that contribute to this disease.
How can someone know that they have periodontitis?
Symptoms are the same as gingivitis but there are some additional signs to detect periodontitis which are.
- Pain or discomfort in the gums.
- Teeth loosening, increased sensitivity, and soreness.
I am confused, could you please tell us the difference between gingivitis and periodontitis?
As already you know about gingivitis, let me explain more about when it leads to periodontitis.
Comparison of gingivitis vs periodontitis:
- The main difference is that gingivitis is reversible while periodontitis is not reversible because of teeth bone loss which cannot be recovered.
- If you are feeling pain while chewing then you think that gingivitis has progressed to periodontitis.
- Are your gums red, swollen, or irritated though your teeth are firmed in place, If yes, then you have gingivitis but if there is tooth loss or inner damage then it has progressed to periodontitis.
- Bad breath is a sign of periodontitis because of excessive bacteria growth in the mouth.
How can we prevent this before it appears in the mouth?
Well, I would suggest the following precautions that everyone should follow to be safe from these diseases.

- Brush your teeth at least twice a day after a meal which is the best time for cleaning teeth and gums because bacteria feed on food particles after the meal and grow.

- Stop smoking, smokers have more chance of getting periodontal disease than non-smokers, also it reduces the success of treatment.

- Use a soft or extra-soft bristled toothbrush.

- Choose an electric toothbrush for maximum cleaning results.

- Reverse periodontal disease by using a natural mouthwash.
- Decrease your stress because in stress body’s immune doesn’t respond very well.

- Take a well-balanced diet that helps your immune system to fight infections. Antioxidant properties of food like vitamin C (Citrus fruits, vegetables, fruit like strawberries, etc) or vitamin E (Nuts, almonds, vegetable oil, soya bean oil, etc) can help to repair damaged body tissues and for gums regrowth.

- Limit sugar.

- Visit at least once a year to your dentist.
And after it appears, what have to do then?
You must consult your dentist to avoid more damage. They will check the deepness of the plaque with a special probe called a dental armamentarium and will remove it.
Could you please recommend to us the best toothpaste for preventing bleeding gums and gingivitis?
I recommend the following toothpaste for bleeding gums but check out this list of “Top 10 best toothpaste for gingivitis and bleeding gums“.
- One 3.4 oz tube of Clean Mint Parodontax Toothpaste for Bleeding Gums, Gingivitis Treatment and Cavity Prevention
- Bleeding gums treatment that breaks plaque apart and kills plaque bacteria
- Antiplaque toothpaste that is three times more effective than sodium monofluorophosphate toothpaste at removing plaque, reversing the effects of gingivitis with regular brushing
- Anticavity toothpaste that keeps your teeth strong
- Gingivitis toothpaste specially formulated to keep the seal between your gums and teeth tight and improve your overall gum health
- Features a cool and refreshing mint flavor to keep your breath fresh
- Brush for two minutes, twice dai
Prices pulled from the Amazon Product Advertising API on:
Product prices and availability are accurate as of the date/time indicated and are subject to change. Any price and availability information displayed on [relevant Amazon Site(s), as applicable] at the time of purchase will apply to the purchase of this product.
Conclusion/Summary
The conclusion is that the answer to the question “What is the difference between gingivitis and periodontitis” is that Gingivitis is the inflammation of the gums while periodontitis is the severe form of gingivitis in which the gum pulls away from teeth, destroys attachment fibers, and supporting bone that holds the teeth. The care of the teeth and gums is very necessary by choosing the best toothpaste or by oral hygiene.






1 thought on “What is the difference between gingivitis and periodontitis, their causes, treatment, and prevention”